The COVID-19 pandemic exposed critical vulnerabilities in global health security, underscoring the urgent need to prepare for future outbreaks. The looming threat of another pandemic necessitates a proactive strategy to predict and preempt potential health crises in the future.
In a panel hosted by the Harvard School of Public Health, scientists and researchers, including CrisisReady Co-Director Dr. Satchit Balsari, shared insights on the innovative tools they are employing to monitor and respond to emerging health crises.
Moderated by Betsy McKay, a global health reporter from The Wall Street Journal, this event delved into the invaluable lessons learned from the pandemic while assessing our level of preparedness for future public health threats.
Moderator
Senior Writer, The Wall Street Journal
Betsy McKay specializes in covering public health and medicine, exploring the impact of diseases and health policies on society. Her articles encompass a wide range of topics, from public health institutions and groundbreaking scientific research to preventive measures and patient care for various global diseases, including heart disease, diabetes, COVID-19, HIV, and tuberculosis.
Speakers
Co-Director, CrisisReady; Assistant Professor, Harvard T.H. Chan School of Public Health, Harvard Medical School; Emergency Clinician, Beth Israel Deaconess Medical Center
Dr. Satchit Balsari’s extensive research focuses on the impact of climate-induced disasters on population health, healthcare infrastructure, and health system resilience. Additionally, his work explores the application of novel technologies and data sources in responding to large-scale public health crises around the world.
Professor of Civil and Environmental Engineering, Stanford University
Dr. Alexandria Boehm’s work focuses on pathogens in the environment and their transmission to humans, as well as developing interventions to reduce disease burdens globally. Her research is focused on critical problems in both developed and developing countries with the overarching goal of designing and testing novel interventions and technologies for reducing the burden of disease.
Director, Center for Communicable Disease Dynamics; Professor of Epidemiology, Harvard T.H. Chan School of Public Health; Director for Science, Center for Forecasting and Outbreak Analytics, Centers for Disease Control and Prevention
Dr. Marc Lipsitch is a Professor of Epidemiology at the Harvard School of Public Health, holding primary appointments in the Department of Epidemiology and an affiliated role in the Department of Immunology and Infectious Diseases. He serves as the Director of the Center for Communicable Disease Dynamics, and also holds the position of Associate Director of the Interdisciplinary Concentration in Infectious Disease Epidemiology.
Laboratory Director, Botswana Harvard AIDS Institute Partnership
Dr. Sikhulile Moyo is a Zimbabwean virologist, currently serving as the laboratory director of the Botswana–Harvard AIDS Institute Partnership and holding a research associate position at the Harvard T.H. Chan School of Public Health. Notably, in November 2021, Moyo and his laboratory achieved the historic milestone of identifying the SARS-CoV-2 Omicron variant as the first to do so.
Reflecting upon the global response to COVID-19 in 2020, the pandemic’s early days were characterized by swift, wide-reaching reactions: borders were closed, businesses halted operations, and neighborhoods were put under mandatory lockdowns. However, despite these measures, the virus continued to spread, pressuring healthcare systems worldwide. Important lessons have been drawn from the initial response, which could shape more effective strategies for future public health crises.

Image: Michael Ciaglo/Getty Images, via WBUR
During the panel, speakers recounted their experiences throughout the pandemic, sharing the lessons they learned and providing insights into how responses to such crises can be strengthened. At the beginning of the pandemic, Dr. Marc Lipsitch stated that there was an urgent need for public health experts, governments, and emergency response organizations to comprehend the geographic distribution and scope of the emergency. This involved not only technological considerations but investing in administrative and epidemiological resources. There was also a need to upscale industrial capacity for testing protocols and adopt case definitions that could detect infections earlier.
According to Dr. Alexandria Boehm, the early stage of the pandemic was marked by insufficient testing capabilities. If more novel infectious disease surveillance networks had been in place, monitoring for SARS-CoV-2 RNA could have offered a more comprehensive view of the virus’s spread. This network was absent in 2020 but now stands as an essential tool for pandemic responses in the future, as is later explained by Boehm.
The COVID-19 pandemic had disparate effects between the Global South and Global North. This was largely due to differences in healthcare accessibility, underlying health conditions, socioeconomic factors, and access to vaccines. The Global South witnessed a significantly higher mortality rate, partly attributed to less developed healthcare systems with fewer resources, leading to suboptimal and delayed care for COVID-19 patients. The toll of the pandemic was exacerbated in developing countries by the prevalence of diseases like HIV/AIDS, malaria, and tuberculosis and the greater proportion of people living in poverty and working in informal sectors. These vulnerable populations, which were typically more exposed to the virus, were often unable to afford isolation or quarantine.
Tackling the Pandemic: Overcoming Obstacles and the Formation of the COVID-19 Mobility Data Network
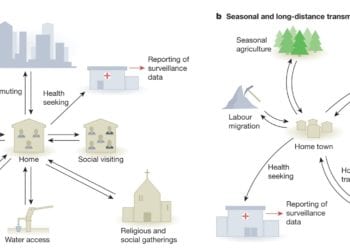
In discussing the Global South’s experience, Dr. Satchit Balsari explained that the lack of adaptability in responses to local conditions was a major issue. Balsari expanded on this by pointing out the lack of creativity in the solutions proposed during the pandemic, especially those that sought to protect vulnerable communities from infection. Measures like physical distancing and isolation, while appropriate in some parts of the world, were simply not feasible in overcrowded urban settings or for families living in close quarters.
Balsari noted that in many parts of the world, lockdowns and school shutdowns disproportionately impacted wage workers and children, plunging them into food insecurity and depriving them of essential resources. In response to these challenges, he called for a more nuanced, contextual approach that would account for the specific circumstances of different communities.
Addressing this critical issue, Balsari collaborated with two of his colleagues: Dr. Caroline Buckee, an epidemiologist and a professor at Harvard T.H. Chan School of Public Health; and Dr. Andrew Schroeder, the vice president of research and analysis at Direct Relief, a humanitarian organization based in California. Together in 2020, they created the COVID-19 Mobility Data Network, a voluntary partnership of over 70 researchers, scientists, and policymakers around the world that worked toward utilizing location data from cell phones in tracking viral transmission. This approach allowed for a more granular understanding of how the virus was spreading and how mobility restrictions were impacting different communities. By incorporating population mobility metrics into epidemiological modeling and reporting, they could ascertain whether the public was still congregating and how commuting patterns had changed.
The work conducted by Balsari, Buckee, and Schroeder’s platform provided important insights, revealing stark differences in community-based mobility patterns during the pandemic. For example, the team found that during lockdown mobility decreased significantly between two boroughs of New York City. “So, for example, we found that mobility had decreased significantly in Manhattan but not in the Bronx,” Balsari said. “And we’re really lucky to work with a public health department that understood that the correct response to that was to provide more support to the Bronx so people could afford to stay at home and not send in a police force to enforce lockdowns, as was happening elsewhere in the world.”
These findings helped shape local responses aimed at reducing transmission of the COVID-19 virus. It was a testament to the power of novel data, namely human mobility data, which allowed public health decisions to be based on concrete information about population movement rather than general assumptions.
“The only way to know whether [non-pharmaceutical interventions] were working was to measure the epidemiological impact […] What we needed to do was to study the impact of actual population mobility on changing epidemiology.”
Dr. Satchit Balsari
Regarding the issue of privacy, Balsari emphasized the importance of full transparency. He noted that the regulations needed to prevent misuse of this data were largely absent outside Europe and parts of California. To protect privacy, Balsari and his team used differential privacy techniques, which add statistical noise to datasets to preserve anonymity.
Privacy concerns related to such data tracking are valid. Addressing these fears requires data anonymization methods and regulations that prevent misuse. It is a delicate balance, ensuring data remains beneficial for public health without compromising individual privacy.
Balsari’s work not only provided meaningful data during the pandemic, but also raised important questions about privacy, transparency, and the need for nuanced public health responses. “These are complex challenges that every society will have to negotiate,” he said. “A year ago, we convened experts from academia, from industry from law and from policy to publish a consensus on how to strike this balance between the availability of data, the resolution at which it should be shared, the conditions under which they can be shared, and these will depend on, again, the trust relationships in society, all this while retaining utility.” The work he and his colleagues accomplished serves as a reminder of how data can be leveraged to inform policy, tailor public health responses to specific communities, and enhance transparency and trust.
The COVID-19 Mobility Data Network gradually transformed into what is now known as CrisisReady. This evolution was driven by the realization that the insights gained from monitoring and interpreting mobility data held significant value for a range of crises beyond COVID-19. CrisisReady is a global network of research scientists and policymakers working together to use mobility data to inform policy decisions during various crises. The initiative continues to provide real-time, data-driven insights to help response organizations understand population movement during events such as natural disasters, humanitarian crises, and public health emergencies. The ultimate aim of CrisisReady is to enhance disaster response and mitigation strategies worldwide.
Wastewater Surveillance: Unlocking New Data Streams for Public Health Response
Throughout the pandemic, the use of various innovative tools and technologies extended beyond mobility data, embracing other viral diagnostic methods and tracking systems to understand viral spread and transmission dynamics. Advanced diagnostic technologies, including next-generation sequencing (NGS) and PCR testing, were pivotal in detecting and identifying the virus. Digital contact tracing apps and data analytics were employed to map out transmission chains and hotspots. Environmental surveillance, such as wastewater testing, provided early warning signs of community transmission. However, despite their significant potential, many of these methods weren’t widely incorporated into public health responses. Their underutilization can be attributed to a range of issues including technological barriers, data privacy concerns, and lack of standardization or coordination.

“Multiple spillovers from humans and onward transmission of SARS …” – PNAS. Available at: https://www.pnas.org/doi/10.1073/pnas.2121644119
Betsy McKay turned attention to Dr. Alexandria Boehm to discuss the potential of wastewater tracking for responding to public health crises. Boehm stated that the global community rallied during the onset of the COVID-19 pandemic to leverage wastewater monitoring for tracking the virus. Prior to 2020, she noted that very little research existed on using wastewater for tracking infectious diseases.
“[…] Before 2020, there was very little research on the use of wastewater for public health or infectious disease surveillance.”
Dr. Alexandria Boehm
As was proven by early COVID transmission modeling efforts, wastewater presents an under-explored reservoir of information. “Wastewater is this composite biological sample,” Boehm said. “It contains feces, urine, sputum, mucus, scabs off the human body, skin cells, anything that goes down the drain, not just the toilet, but the shower or the sink. And so if you have the genomic sequence of the threat that you’re interested in, whether it’s an old threat or a new threat, you can apply an assay to wastewater to look for nucleic acids for that threat.”
Wastewater provides an all-inclusive sample as it captures excretions from everyone in the contributing population, which can range from thousands to millions of people. In the U.S, wastewater treatment plants serve approximately 75% of the population. However, Boehm pointed out that this approach might not be universally applicable, as in many low- and middle-income countries, centralized wastewater treatment plants may be absent.
Boehm then brought the conversation back to the importance of trust. She stated that trust in the efficacy of wastewater surveillance is crucial to using it in public health response.
“Building on this theme of trust, one of the really important things about the use of wastewater surveillance to track new threats or old threats and inform public health it is you can’t just make the measurements and inform public health,” she said. “You have to have a trusting relationship with public health so that they trust you and they understand this data stream and how this data stream can be used to inform their response to the pandemic and how it complements the sorts of data streams that they’re used to seeing.”
Advancing Genomic Sequencing: Insights on Tracking Variants and Enhancing Pandemic Response
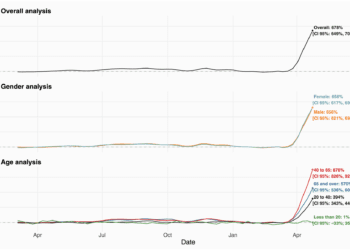
In the conversation, Virologist Dr. Sikhulile Moyo explained the vital role genomic sequencing has played in the global response to the COVID-19 pandemic. He underscored that his lab’s discovery of the Omicron variant at the Botswana-Harvard AIDS Institute Partnership highlights the value of genomic surveillance. It allowed the world to prepare for potential surges due to the detection of significant genetic changes in the virus. The ability to quickly share data and maintain transparency from scientists in Southern Africa were key to informing the world about the impending challenges.
Moyo pointed out that the genomic surveillance data also helped predict the possible impact of these mutations, such as potential vaccine escape or increased transmissibility. In response, interventions were quickly implemented, such as renewed social distancing and a boost in vaccination programs. While travel bans were implemented in response to the variant’s discovery, he suggested that such measures were less effective and could be harmful.
“I think COVID-19 has helped us to see the power of genomic sequencing.”
Dr. Sikhulile Moyo
Moyo stated that a better pandemic response mechanism needs to be in place, emphasizing that transparency, data sharing, and scientific collaboration are crucial. “We saw that the importance in terms of Public Health response is transparency. We need to share our data and collaborate with other scientists,” he said. “[The Omicron discovery] was critical in the development of a new adapted Omicron-adapted vaccine. So we see that this is important to monitor this virus, to warn as much as possible, but it’s important that the response should be commensurate with the threat levels that the variants pose.”

Image: Harvard School of Public Health
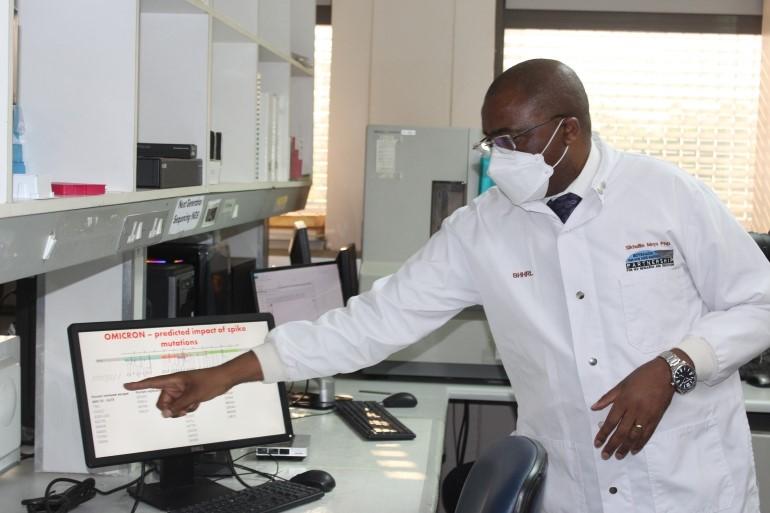
Image: Think Global Health
Looking forward, Moyo argued that the power of genomic sequencing brought to light by the COVID-19 pandemic offers a glimpse into the possibilities of precision public health. It can help monitor the virus’s evolution and adapt vaccines accordingly. With tools to link genetic mutations and changes in epidemiology, health officials can evaluate the effectiveness of vaccines, enhance clinical guidelines, and make informed decisions about public health measures. Diagnostic kits, therapeutics, and the ability to analyze potential phenotypic changes all benefit from genomic sequencing, illustrating its critical importance in the ongoing fight against the virus.
Data Integration for Advanced Forecasting and Outbreak Analytics at the CDC
Dr. Marc Lipsitch, the Director of Science for the newly established CDC Center for Forecasting and Outbreak Analytics, discussed the essential role of data integration in managing and mitigating the impacts of pandemics. He emphasized the value of harnessing a variety of data sources to drive short-term forecasts, long-term scenario projections, and analysis that can better inform policy. These include decisions on testing, isolation strategies, and the potential impacts of closing borders.
“[…] We’re really working within the Center for Forecasting and Outbreak Analytics to find more ways, particularly to combine high-quality clinical data with high-quality genomic data, which I think those two together are much more powerful than each of them individually.”
Dr. Marc Lipsitch
Highlighting a case study from the CDC’s efforts during the Omicron wave, Lipsitch explained how the center combined genomic data with high-quality clinical data to assess the severity of the variant. He noted, “we were able to produce a preprint within about a month of the initial contact that Dr. Walensky, the CDC director, was able to publicly share that indicated that there was a substantially lower severity per case. It was a tremendously destructive wave. It was not as destructive as it would have been at a Delta level of severity.”
This assessment played a pivotal role in informing public understanding and planning measures during the Omicron wave. Lipsitch also highlighted the power of combining clinical data with genomic data, asserting that their joint application can yield insights much more potent than when each set of data is considered individually.
Moving forward, Lipsitch indicated that the lessons learned from the COVID-19 pandemic and the value of genomic sequencing can be applied to broader disease prevention and outbreak management.
The COVID-19 pandemic has been a watershed moment for global health. It has exposed critical vulnerabilities in public health systems around the world and has highlighted the importance of international cooperation, all while teaching us valuable lessons that will serve as a foundation for future public health responses.
Among the many lessons learned from the pandemic is the importance of early detection and response, as the virus spread rapidly due to delayed detection. Investments in early warning systems and rapid response mechanisms are critical for containing outbreaks before they escalate into pandemics. The crisis also underscored the need for global coordination, especially as it pertains to international public health threats. Rapid viral spread across borders requires collaborative efforts to share information, align responses, and develop vaccines and treatments in a timely manner. The pandemic also laid bare the inadequacies of public health infrastructure, highlighting the need to invest in enhanced surveillance, testing, contact tracing, and other public health measures.
Echoing the sentiments of the panel, trust is essential for public health interventions to be effective, and health crises can be mitigated by empowering local communities to take action. In addition to this, investing in innovative technologies, novel data, and new methods of viral surveillance are essential to prepare for future public health crises.
For more information about the panel, you can visit the event webpage on the Harvard School of Public Health website. Alternatively, you can watch the entire discussion online here.